Considerations to Create a COVID-Safe Home: Air Treatment and Screening Guests
Are you considering an in-person gathering with family, friends or colleagues?
A social gathering without taking COVID-safe precautions is more dangerous than riding in a car in snowy, icy conditions with a driver who is legally intoxicated.
Summary
Your family and guests are more likely to be safe if you invite people who are not going to more than one gathering. Invite people who agree to not go to more than one gathering in a 2 week period.
Read CDC COVID-Safe guidelines that apply to holiday gatherings. Decide what you can do to mitigate the reality that all people are not going to wear a mask all the time they are gathered.
Install an air filter in your HVAC that provides maximum filtration. MERV 13 at least. Check with your HVAC service company.
Limit the number of people in a room to ensure you have at least 100ft2 open floor space for each person. Don’t crowd the room. Allowing 200ft2 per person is 3 times better.
Give each person a clean washcloth to hold or put in pocket to cover their face if they need to sneeze or cough.
Purchase, rent or borrow at least 4 True HEPA air filtration machines with a CADR of 180ft3 per minute if you intend to clear a 500ft2 room with a 10 ft ceiling. Using 2 air filtration machines is 4 times better than no machines.
Increase the heat in your house before guests arrive if the weather is cold. This way additional ventilation by opening windows will cool the house more slowly. Consider extra heaters and be sure guest bring warm clothing if you open windows.
Use fans in the room to mix and dilute the air people exhale. You need a mild breeze everywhere to do this. Oscillating fans work great
Make it a rule and tell every guest to not tease or ridicule people who chose to wear a mask. A face covering protects other people, not you. A filtration mask that filters 90 to 95% of particles will protect you.
Ask everyone coming to a gathering to complete a comprehensive screening before coming to the gathering. Ask people with a moderate, or high risk to not come. Adhering to a comprehensive screening is one of the the best things you can do to keep your guests and family safe.
Limit the gathering to no more than 2 hours, to as few people as possible, and ventilation that is at least 120 ft3 per minute per person.
CLICK HERE to start your anonymous COVID-19 Comprehensive Risk Estimate Screening. Or click on the button below.
The CDC provides good options but many people won’t follow them.
Public health officials and the CDC are publishing general precautions for holiday gatherings and event safety. These are quite general.
The ability to create a COVID-Safe home over the holidays is a matter of learning what steps you can take to reduce risks of infection and then taking those steps. What is the acceptable level of risk in one gathering? The CDC is vague on this issue probably because each person’s answer depends in large part on the community where you live, the physical characteristics of your home, the behavior and state of health of the people in your home, and the behavior and state of health of people you may invite. People assume friends are equally safe because they share other similar values. The risk in a specific case may be relatively easy to predict if you are an engineer or epidemiologist with all the data but is impossible to predict in generality.
People creating a gathering have many things to consider. As a minimum, they should read what the CDC and public health authority recommend. In reality, people may adhere to all it, part of it, or none of it. But if you poll your active patients and friends you may discover that few if any intend to require guests in their home wear masks at a gathering of family and friends.
Recommendation: Read CDC COVID-Safe guidelines that apply to holiday gatherings. Decide what what you can do to mitigate the reality people are not going to wear a mask.
Additional options based on evidence and science than will reduce risk
A gathering in a 20 by 25 foot room (500ft2) with a 10 foot ceiling has a volume of 5000 cubic feet of air. The probability of one person being infected is conservatively between 0.017% and 0.32%. That includes people who have clinical and pre-clinical symptoms, or people who are asymptomatic. In Oregon, there is 1 chance in 312 that a person is infected. That may sound safe but how safe is it really for the rest of us?
One infected person in an enclosed 500ft2 space for an extended time without COVID-Safe precautions will almost certainly infect at least 50% and potentially everyone. That becomes a serious problem because those people can infect everyone in the next gathering. Before you know it, one person’s infectivity in one gathering has infected 5 more people. If each of those 5 people go to separate gatherings, they can infect up to 125 more people. And those people can infect 625 in subsequent gatherings.
Recommendation: Invite people who agree to not go to more than one gathering in a 2 week period. People are not considered infected if they have no symptoms after 14 days if they take COVID-Safe precautions..
During fall and winter many people catch cold or flu. It is important to get a flu vaccination. While not 100% certain, getting any flu symptoms means you should definitely consider whether you may be infected with SARS-CoV-2. Getting a flu vaccine doesn’t create immunity. It means you have a lower risk of becoming infected with the flu. It means you are more likely to be infected and have COVID-19 if you have any symptoms that are like the flu.
Recommendation: Get a flu vaccination. That way, symptoms of the flu are probably not the flu.
A room where family members gather must have air that is well mixed, meaning the air should not be still. There should be fans that move the air in manner similar to a gentle breeze. If there is high humidity and low temperature then a live virus can live for many hours and not fall to the ground. The air needs to be still in order to fall to the ground. There is not much chance of that happening in an active room with people moving around. On the other hand, a room that has low humidity and a high temperature is likely to dry out a virus-carrying droplet. That particle is not going to fall to the ground and can travel long distances and move all over the room in 5 minutes.
CO2 monitor
Gathering rooms should be ventilated, meaning fresh air should replace room air at rate such that the CO2 levels remain at a background level of about 400 parts per million. That air movement increases the amount of fresh air people are breathing. One way to insure you have adequate fresh air supply is to purchase a CO2 level monitor. Many of these devices also measure temperature and relative humidity. Try to keep the temperature above 70F and humidity below 35%.
Recommendation: Purchase a CO2 monitor and make sure the CO2 level in the room does not increase by turning up the heat and opening a window.
Heating, ventilation and air-conditioning (HVAC) systems for a gathering space should be running continuously. At the very least the air circulation fan should be turned on. The air filter in a standard HVAC is typically a MERV 8. If possible, the air filter slot in the HVAC should fitted with a MERV 13 filter. (Check with the HVAC service company to be sure a MERV 13 or better will work efficiently and not cause harm to your HVAC system.) If your house is heated with radiant heat, wall heaters, radiators etc. you will definitely need a lot more ventilation and filtration.
Recommendation: Install an air filter in your HVAC that provides maximum filtration.
According to the EPA, natural ventilation is an option. Open more than one window or door, if possible. Ventilation can be further increased through cross-ventilation, by opening windows (or doors) at opposite sides of a home (but preferably not directly opposite of each other), and keeping internal doors open. Opening the highest and lowest windows in a home at the same time (especially on different floors) can also help to increase ventilation. For double-hung windows (the most common type), opening the top sash of one window and the bottom sash of another also encourages ventilation. Even when using a single window, partially opening both the top and bottom sash can help improve ventilation. For additional ventilation, multiple fans can be used, pushing air out of one window and drawing it in from another. If a single fan is used, it should be facing (and blowing air) in the same direction the air is naturally moving. You can determine the direction the air is naturally moving by observing the movement of drapes, holding a light fabric, or dropping paper clippings and noting which direction they move. The direction the air is blowing (in or out of the home) from a particular window or door may change at times, especially on windy days. If these changes are frequent, try moving the fan to another location. Also, you may not need to use a fan on windy days. If you live in a two story house, have the gather upstair, open a downstairs window
Air exhaust and replacement fan
Recommendation: Install and air exchange ventilation system in a window to insure CO2 levels do not increase and room air is replaced with outside air.
Physical distance is critical. You should keep at least a 6 foot distance between people at all times. It is important to keep in mind that we don’t know the difference of infectivity between a person who has symptoms and an infected person with no symptoms. We do know that people who are singing, talking loudly, coughing or sneezing will exhale as much as 100,000 times more virus in a single breath than a person sitting and engaged in normal conversation. So we need to assume that any infected person can infect others whether they believe they are infected or not. In any room, you should have no more than one person per 100ft2 of the room. That means no more that 5 people can be in a room that is 500 square feet. Ideally you want no more than 3 to 4 people in a 500 ft2 room.
Recommendation: Limit the number of people in a room to insure you have 100ft2 for each person. Don’t crowd the room.
Recommendation: Give each person a clean washcloth to hold or keep in their pocket to cover their face if they need to sneeze or cough.
Physical distance is critical. You should keep at least a 6 foot distance between people at all times. It is important to keep in mind that we don’t know the difference of infectivity between a person who has symptoms and an infected person with no symptoms. We do know that people who are singing, talking loudly, coughing or sneezing will exhale as much as 100,000 times more virus in a single breath than a person sitting and engaged in normal conversation. So we need to assume that any infected person can infect others whether they believe they are infected or not. In any room, you should have no more than one person per 100ft2 of the room. That means no more that 5 people can be in a room that is 500 square feet. Ideally you want no more than 3 people in a 500 ft2 room.
Recommendation: Limit the number of people in a room to insure you have 100ft2 for each person. Don’t crowd the room. $200ft is 3 times better that 100ft2.
Recommendation: Give each person a clean washcloth to hold or put in pocket to cover their face if they need to sneeze or cough.
Without question you need at least 6 air exchanges per hour. Six is for a physician’s standard examination room. Ideally you want 13 air exchanges. This is for airborne infectious disease isolation room. Fifteen air changes per hour is closer to the requirements for an airborne infectious disease isolation room in a hospital. To accomplish that you need to exchange inside air with outside air and/or filter the air at the same rate as you exchange it with the outside.
Air filtration device
The volume of a 500 square foot room with a 10 foot ceiling is 5000 cubic feet. To get 10 air exchanges you need to calculate the exchange rate in cubic feet per minutes. So 5000 cubic feet divided by 60 minutes is 83 cubic feet per minute. However there needs to be a stable rate. It is important to remove the air equally throughout a room and not in just one area. So practically speaking you may need more than one air-exchange and/or filtration system for a room filled with people.
A stand alone air filtration unit is useful if you can’t ventilate air during extremely cold weather. You would definitely need this if you have wall mounted electrical heat. The CDC considers standalone air filtration to be an adequate substitute for air-exchange. More air filtration means less risk of infection from aerosolized droplets.
Stand alone air filtration systems include HEPA, TrueHEPA and ultraHEPA types. Medical grade filtration is TrueHEPA or ultraHEPA. The clean air delivery rates (CADR) of a filtration unit varies in cubic feet of clean air per minute.
A stand alone filtration system with TrueHEPA providing a CADR of 300 ft3 per minutes can clear the air in a 3000 ft3 room in 10 minutes (or a 5000ft3 room in 16 minutes.) However placing one standalone device on one side of a room will not clear the air as quickly in the opposite corner of the room. Placing 4 devices, each on opposite walls of the room will help insure air is exchanged equally throughout the room. Using 4 filtration machines with a CADR of 300ft3 per minute will clear a 5000ft3 room in 4 minutes. That will be more certain if the air is well mixed and people stay 6 feet from each other and speak at conversational speech levels, about 50 decibels.
Air wall
Recommendation: Purchase, rent or borrow at least 4 True HEPA air filtration machines with a CADR of 300ft3 per minute if you intend clear a 5000ft3 room for 6 people. A ultraHEPA device in better.
Virus-carrying droplets that are exhaled by an infected person dry out in a few minutes if the humidity is about 35% and the temperature is 70 degrees. The aerosolized droplets can float for several days if the air is turbulent. However, aerosols don’t live forever. About 50% of the viruses that are exhaled die each hour in a warm low humidity room.
Air filtration is a violent process subjecting a virus to wind shear, impaction and desiccation. A virus will go “splatt” and die before it leaves a filtration device operating a moderate to high speed. A filtration device running at high speed is not be more effective than moderate speed in a room with 2 or 3 people who are seated.
An airwall is a fan that is shaped like a tower with a vent that is about 4 inches wide and 48 inches tall. Such a fan will mix the air very well but also redirect conversation speech away from 2 people talking face-to-face.
Cotton washcloth
Wearing a mask is important to slow and reduce the spread of airborne virus-carrying droplets. Someone coughing without covering their face is practically a “smoking gun.” In general, your mask will help protect other people if you are infected but it will not protect you from inhaling an infectious quantity of virus if others are infected. Wearing a face covering is important if you are in close proximity to others, and people are talking loudly. To keep yourself safe, you need a mask that filters at least 85% and preferably 90% of airborne particles. Otherwise the mask simply blocks spray and therefore the distance in which you spread the virus if you cough, sneeze or speak loudly. People standing and talking loudly exhale 10,000 times more virus that people seated and talking softly. Ideally a two way filtration mask should be sealed firmly to your face. Men must remove their beards to seal most masks effectively. Effective filtration masks are tight and well fitted.
Recommendation: Make it a rule and tell every guest to not tease or ridicule people who choose to wear a mask.
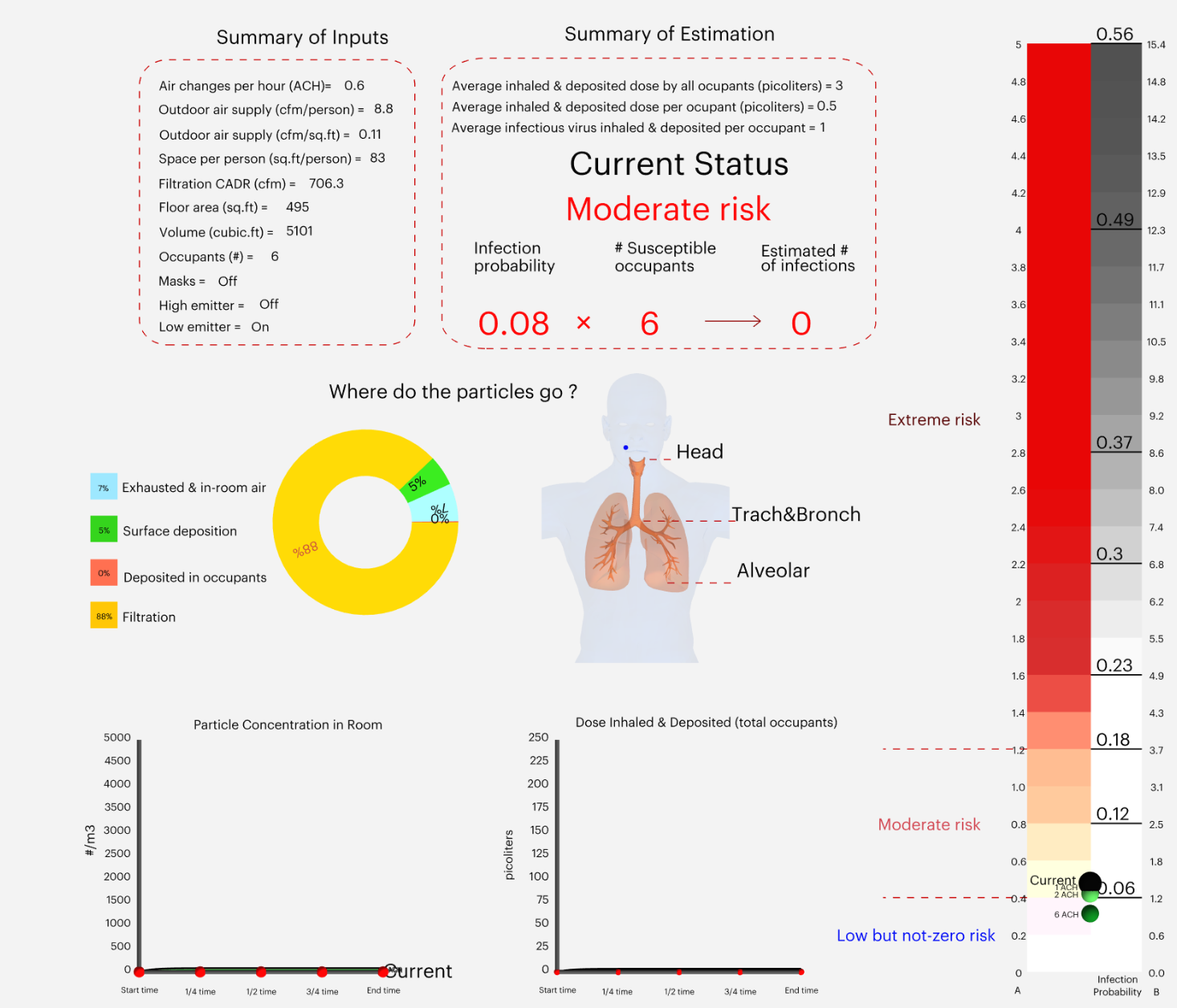
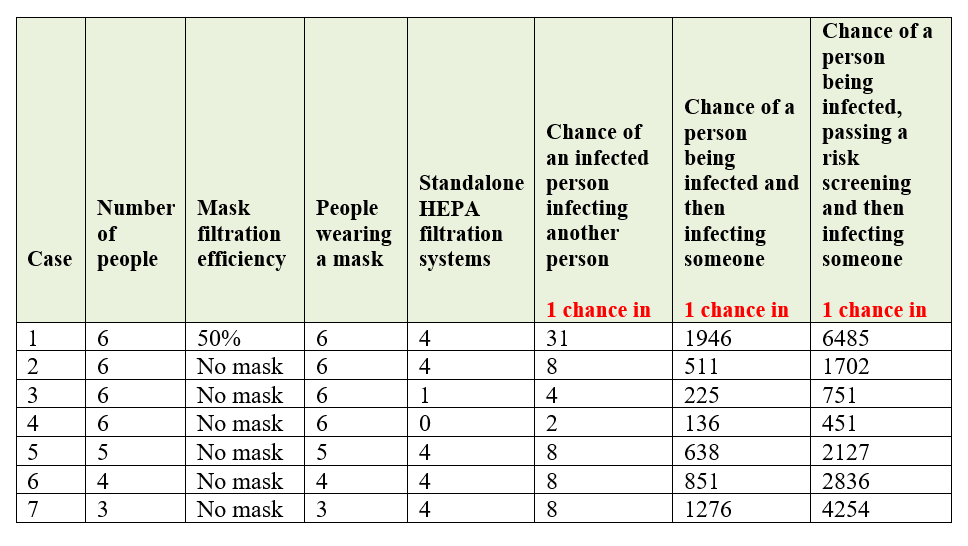
So what are the odds of becoming infected if:
you gather 6 people in a 500ft2 room with a 10ft ceiling for 2 hours,
everyone is standing up and speaking loudly,
there is an HVAC that exchanges 70% of the air per hour,
there is 50ft3 of ventilation per minute of outside air,
there are a varying number of standalone HEPA filtration devices with a CADR of 180 ft3 per minute each,
nobody wears a mask or everybody wears a mask that has a 50% filtration efficiency,
people stay t least 6 feet from each other, and
there are fans in the room used to mix and dilute the exhaled air.
With respect to the above case, if we assume one person is infected and doesn’t know it, and nobody wear as mask, there is 1 chance in 31 that an additional person will become infected. Likewise, there is 1 chance in 4 that a person will become infected if there is only 1 properly placed HEPA air filtration system and nobody wears a mask in the room. There is 1 chance in 2 (50%) that someone will become infected if there is no air filtration and no one wears a mask.
How safe is 1 chance in 31? There is very good chance (97.0%) that no one in this gathering will be infected. In most cases, probability is presented in ways that are difficult for many people to understand. For example, what does 1 chance in 1702 actually mean? Think of number between 0 and 1703. Do you think another person can guess that number? The chance is nearly impossible. However, one way to be very conservative is to think in terms of an order of magnitude. An order of magnitude is usually 10% of the original value. We can be certain that the probability is no more that 1 chance in 170. That is very close to zero.
Airborne and aerosol COVID-19 infection risk estimators provide a reliable estimate of relative risk
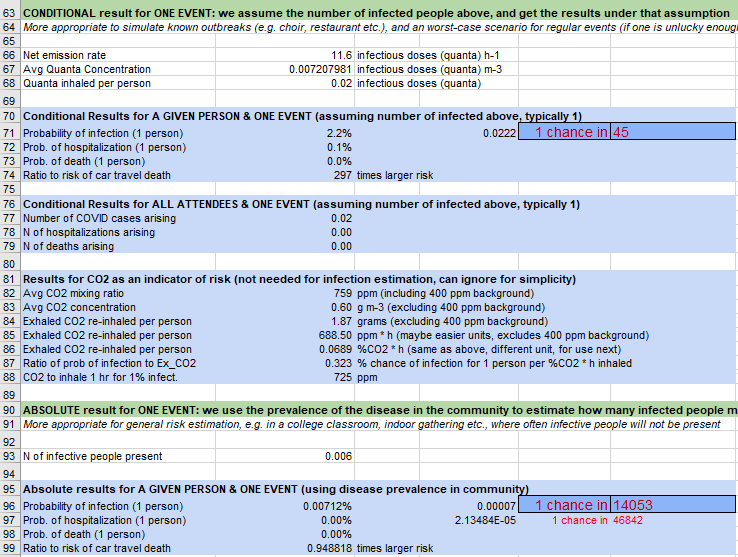
Example 1. COVID-19 Aerosol Infection Risk Estimator (unvacinated).
Example 2. Exposure Risk Estimator for COVID-19 (unvacinated).
Table 1 presents data generated by a COVID-19 Aerosol Infection Risk Estimator adapted by Mentor Research Institute for private psychotherapy practice. This model will work in a one room office. Similarly, these estimator can be used to estimate infection risk in a family or living room.
Table 1. Relative Risk of Infection Table using the COVID-19 Aerosol Infection Risk Estimator (unvacinated).
The Relative Risk of Infection. This table is based on basic assumptions including a 500ft2 box shaped office, HVAC with Merv13 filtration, 70% ventilation/hour, 6 foot separation, loud conversation while standing (less that 60 decibels), CADR of 180ft3/min. Passing a risk screening is defined as low. risk.
The chances of infection is the relative risk table above are estimates. The model used here is based on a standard model of aerosol disease transmission, the Wells-Riley model. It is calibrated to COVID-19 based on recent literature on quanta emission rate. According the the developers, “…this is NOT an epidemiological model, rather can take input from such models for the average rate of infection for a given location and time period.”
While the risks in Table 1 are not absolutely accurate they are almost certainly accurate with an order of magnitude. For example, consider the risk of 1 chance in 1702. Within an order or magnitude of one decimal point the odds of becoming infected if you gather 6 people in a 500ft2 room with a 10ft ceiling, for 2 hours, have an HVAC that exchanges 70% of the air per hour, has additional ventilation of 50ft3 per minute of outside air, no one wears a mask, you maintain 6ft of separation, and you have 4 properly placed HEPA filtration devices, there an absolute combined risk of 1 chance in 170 (compared to 1 chance in 1702) that someone will be infectious and then infect another person. Those a very good odds that you won’t become infected.
Additionally this model provide a highly accurate relative risk data. Meaning, having 4 filtration devices are at least 2 times safer than 1 device. And having 4 devices is 4 times safer that having no devices.
Recommendation: Accept that air filtration can help reduce the risk but is not a substitute for limiting the number of people per room, reducing the volume of speech, and insuring there is adequate ventilation.
It is worth noting that a gathering where guests accurately honestly pass the systematic screening below will provide a high level of protection. Wearing a mask and using a HEPA air filtration system provides the best protection.
You might ask, what else can be done to reduce the risk of infection. People sitting and talking as a normal conversation level will reduce the risk even farther. As much as 4 times lower.
Lastly, it is important to not allow someone in your gathering who may be pre-clinical or asymptomatic. The best way to insure that is that all guests agree to isolate for 14 days. If you can’t do that then you need to systematically screen people you let into your house. Their is no easy way to do this because you need to eliminate the risk to yourself, your family and friends by having zero tolerance for behavior and symptoms that may (and may not) be associated with a moderate or high risk of becoming infected with COVID-19. The reason this is hard is because you have set clear expectations and draw the line with people who do not meet those expectations. One way to resolve this is to debate the issue based on your opinions and what you think is a safe set of criteria. Or you can rely on more systematic screening based based on evidence, research and good clinical practice.
COVID-19 comprehensive infection risk screening reduces infection and health risk significantly
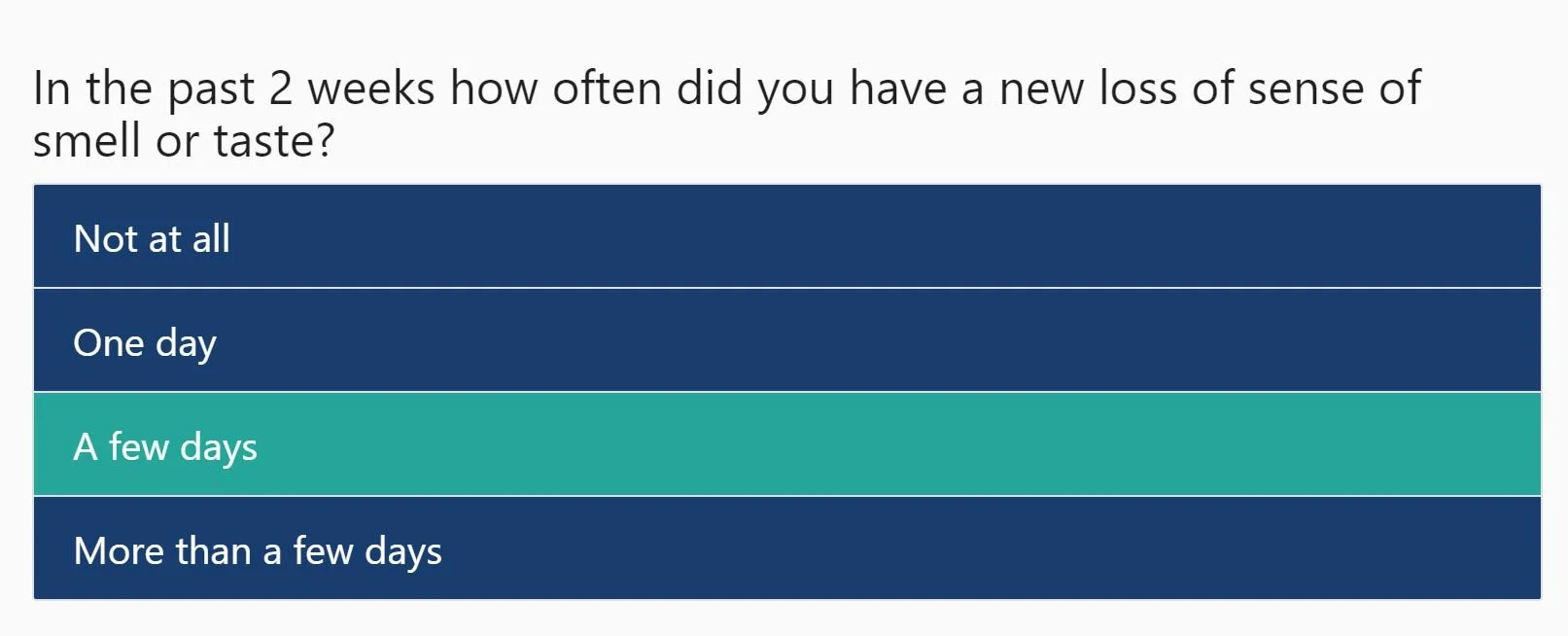
A COVID-19 comprehensive risk screening was created as part of a training developed by Mentor Research Institute in July 2020. The screening questionnaire has evolved and is now available online. In that screening there are 4 categories of risk.
Health risks and specially those of a weakened immune system.
The risks that are the result of a type of activity,
The risks that are results of whom and what behavior you are exposed to,
The risks that physical symptoms are from an active COVID-19 infection.
Here is a link to access an anonymous screening for COVID-19 in that system.
CLICK HERE to start your Anonymous Screening
Example Question in a Comprehensive COVID-19 Infection Risk Estimator
After completing 46 questions the results are displayed for you to save or print. What do the results of the COVID-19 Comprehensive Risk Screening mean? The screening process and results are very straightforward. The results are intended to provide conservative estimates of risk. The risk levels are mild, moderate, high and very high. The questionnaire scoring is designed to screen out high numbers of people who are not infected because their symptoms, but also those who engage in behavior and s lifestyle them places them at greater risk. For example, particular activities and situation can be used identify people who are not adhering to personal protective behaviors that reduce risk of infection. To learn more and to gain more detailed information about the comprehensive infection risk estimator you could consider joining the COVID-19 discussion forum at www.OregonTherapyForum.com.
Recommendation: Ask everyone coming to a gathering to complete a comprehensive screening before coming to a gathering. You have to decide what level of risk you are willing to accept if you are the host.
Recommendation: Definitely wear a mask indoors if a room does not have adequate air treatment, people do not keep social distance, and those people have a moderate to very high risk based on a comprehensive screening.
Can I afford to get COVID-19?
NeuroCOVID Symptoms
What are the chances that elderly people will die from COVID-19? It can cost you your life or your long term health. What many people fail to consider about COVID-19 is that not dying from COVID-19 does not mean you fully recover. The near and long term health impacts of COVID-19 can be significant, may disable you in several different ways for weeks, months or years, and require ongoing medical care. Physicians are now finding COVID-19 patients have damage not just to their lungs but also to their heart, kidneys, liver, brain and/or gut. If you are hospitalized for more than 3 days the chance that you may have mild to severe heart damage is 1 chance in 2 (50%).
Image of Heart and Circulatory Damage cause by COVID-19.
There is a financial price to pay should you become infected and seriously ill. While you can survive being hospitalized there is a significant bill for the care you receive. The costs are greatest on the first day of intensive care. Mechanical ventilation is about $10,000 the first day and without mechanical ventilation the cost is about $6,500. In round numbers, starting on day 2 the cost of mechanical ventilation is about $4,500 per day and without mechanical ventilation the cost is about $3,500 dollars.
People who have COVID-19 can end up staying in the hospital for weeks or months. Those discharged may have a long road to recovery including physical therapy, respiratory therapy, physician check-ups, and brief to long term treatment with medications.
Recommendation: Discuss with your family and guests that the cost of hospitalization and even infection without hospitalization could bankrupt a family.
A social gathering without COVID-safe precautions during the holidays is more dangerous than riding in a car in the snow with a driver who is legally intoxicated. For this reason, carefully providing air treatment (ventilation and filtration), sanitization of surfaces, requiring physical distance, and comprehensive screening guest in advance will provide a COVID-Safe home with very high level of certainty.
References
Effectiveness of Air Cleaners for Removal of Virus-Containing Respiratory Droplets: Recommendations for Air Cleaner Selection for Campus Spaces, https://shellym80304.files.wordpress.com/2020/06/air-cleaner-report.pdf, May 2020.
Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. The New England Journal of Medicine, https://pubmed.ncbi.nlm.nih.gov/32182409/ April 2020.
Daily cost of an intensive care unit day: The contribution of mechanical ventilation , Critical Care Medicine, https://pubmed.ncbi.nlm.nih.gov/15942342/ . July 2005.
Effectiveness in In-Room Air Filtration and Dilution Ventilation for Tuberculosis Infection Control. Air & Waste Management Association. https://pubmed.ncbi.nlm.nih.gov/8806221/ 1996.
Herd Immunity and Implications for SARS-CoV-2 Control. JAMA Insights, https://jamanetwork.com/journals/jama/fullarticle/2772167. October 2020.
Ultrasound shows Impact of COVID-19 on the Heart. https://www.mountsinai.org/about/newsroom/2020/ultrasounds-show-impact-of-covid19-on-the-heart-pr , October 2020.
Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19), JAMA, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7385689/ July 2020.
Long-Term Effects of COVID-19, CDC, https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects.html , September 2020.
Re-open and Maintain Your In-person Mental Health Practice Responsibly During the COVID-19 Pandemic (Training), Mentor Research Institute, https://www.mentorresearch.org/covid-19-practice-training. July 2020.
COVID-19 Safe Air Quality for Psychotherapy Practice During the SARS-CoV-2 Epidemic (Training), Mentor Research Institute, https://www.mentorresearch.org/covid-19-safe-air-quality-psychotherapy-practice, November 2020.
Coronavirus (COVID-19): Infection control and prevention measures, https://www.cochranelibrary.com/cca/doi/10.1002/cca.3215/full, November 2020.
Signs and symptoms to determine if a patient presenting in primary care or hospital outpatient settings has COVID‐19 disease, https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD013665/full , July 2020.