Biological Feedback Loops and Relationship Breakdown: Psycho-Neuro-Endocrine Dynamics that Escalate, Sustain, Block Repair, and Repair
Mentor Research (2025)
Abstract
This paper examines the neuroendocrine foundations of relationship strain, conflict escalation, and emotional disconnection between romantic partners. Drawing on research across psychoneuroendocrinology, affective neuroscience, and couple therapy, it argues that biological feedback loops, particularly involving cortisol, testosterone, estrogen, progesterone, oxytocin, dopamine, and serotonin, strongly influence relational stability. Female hormonal cyclicity introduces periodic changes in stress sensitivity, empathy, and affiliative drive that can heighten vulnerability to conflict. Male hormonal systems, by contrast, promote short-term dominance and withdrawal responses that amplify misunderstanding. These differences interact to sustain maladaptive feedback loops that erode trust and intimacy. Clinical implications include timing interventions with hormonal rhythms, reducing cortisol–oxytocin antagonism, and reframing conflict as a physiological rather than purely psychological event.
Introduction
Relationship distress has traditionally been conceptualized in psychological, social, or communicative terms. However, a growing body of evidence suggests that intimate partnerships are also profoundly shaped by neuroendocrine systems that evolved to balance survival, reproduction, and social bonding [1][2]. Each partner brings a biologically calibrated stress and attachment system that interacts dynamically with the other’s. When these systems synchronize, they promote empathy and regulation; when misaligned, they amplify stress, misinterpretation, and defensive behavior.
The concept of biological feedback loops, recurrent interactions between hormones, brain networks, and behavior, offers a powerful explanatory lens for understanding chronic relationship tension. Hormonal responses are not random but cyclic, predictable, and modifiable [3][4]. This paper explores how sex-linked hormonal patterns influence escalation, recovery, and intimacy, emphasizing how female endocrine cyclicity often sustains conflict longer and delays relational repair.
The Hormonal Architecture of Intimate Behavior
Cortisol and the Stress Axis
Cortisol, the principal stress hormone, orchestrates energy mobilization and vigilance through activation of the hypothalamic–pituitary–adrenal (HPA) axis [5][6]. In moderate doses, it enhances focus and short-term coping. In chronic conflict, however, sustained cortisol elevation suppresses oxytocin, serotonin, and gonadal hormones, undermining both attachment and sexual function [7][8].
In intimate contexts, cortisol surges during perceived threat or criticism. When couples engage in hostile exchanges, both partners’ cortisol levels rise and often synchronize, amplifying physiological arousal even when one partner attempts calm [9]. This reciprocity can transform a brief argument into hours of emotional distance. Repeated cycles of stress lead to allostatic overload, blunting empathy and decreasing reward sensitivity.
Testosterone and Dominance Motivation
Testosterone promotes assertiveness, competitiveness, and reward seeking [10][11]. In men, transient increases occur during competition and sexual interest, enhancing confidence and risk-taking. During relationship conflict, these surges can translate into defensiveness or aggression. When cortisol simultaneously rises, the dual-hormone hypothesis predicts unstable dominance, assertive but poorly regulated behavior [12].
Paradoxically, stable pair-bonding and fatherhood suppress baseline testosterone [13]. This decline enhances nurturing behavior but reduces tolerance for sustained stress. Under chronic relational tension, cortisol inhibits testosterone synthesis, producing fatigue and withdrawal. Men in this state often appear emotionally disengaged, though physiologically they are depleted rather than indifferent.
Estrogen, Progesterone, and Female Affective Cyclicity
Estrogen and progesterone regulate the female reproductive cycle but also influence mood, energy, and cognition [14]. Estrogen enhances serotonin and dopamine transmission, promoting optimism and sociability. Progesterone, dominant in the luteal phase, can increase sensitivity to threat and decrease serotonin. The premenstrual decline in both hormones contributes to irritability and emotional volatility [15][16].
During the follicular phase (approximately days 7–14), high estrogen supports affiliative motivation and sexual receptivity. In the luteal phase, falling estrogen and progesterone shift the body toward vigilance and protection. These shifts can transform the same partner from emotionally open to reactive or withdrawn within days [17].
Oxytocin: The Bonding Hormone
Oxytocin facilitates trust, empathy, and attachment [21]. Released during touch, eye contact, and sexual intimacy, it reduces amygdala reactivity to social threat and attenuates cortisol [22]. However, oxytocin’s effects depend on context, it amplifies social salience, making positive experiences warmer but negative exchanges more painful [23]. When cortisol levels remain high, oxytocin’s soothing effects diminish, and affectionate gestures fail to reduce distress [27].
Dopamine and Reward Conditioning
Dopamine governs motivation and reinforcement [31]. In relationships, dopamine mediates the “spark” of attraction and the pleasure of resolution after conflict. Yet intermittent conflict followed by reconciliation produces a variable-reward schedule identical to addictive reinforcement [32]. Couples can become unconsciously conditioned to oscillate between argument and relief, mistaking volatility for passion.
Serotonin and Emotional Stability
Serotonin regulates impulse control and mood [19]. Low serotonin, common under chronic stress or sleep deprivation, heightens reactivity to rejection and anger [33]. During the late luteal phase, serotonin depletion magnifies irritability, contributing to premenstrual dysphoric disorder (PMDD) [39]. When both partners are stressed, reduced serotonin and elevated cortisol form a biochemical substrate for escalation: the body primes for defense, not dialogue [34].
Interaction Loops and Conflict Escalation
The Female Stress-Sensitivity Loop
The interplay between estrogen, progesterone, and cortisol forms a recurrent loop that heightens female stress sensitivity. Estrogen suppresses cortisol, but when estrogen drops, cortisol reactivity increases [14]. This explains why stress and criticism feel more intense in the luteal phase [15].
Female partners often initiate repair after conflict, but during high-cortisol states they experience decreased oxytocin sensitivity, making reassurance ineffective. The resulting frustration (“Why don’t I feel comforted?”) leads to further cortisol release, creating a self-reinforcing loop of vigilance and dissatisfaction [27][28].
The Male Competition-Withdrawal Loop
Men’s physiological response favors fight-or-flight. A rise in testosterone promotes dominance; prolonged stress elevates cortisol, which then suppresses testosterone [29]. As stress continues, motivation shifts from engagement to withdrawal. Partners perceive this withdrawal as emotional abandonment, which increases female stress arousal and pursuit [30]. The classic demand–withdraw cycle thus emerges from endocrine reciprocity, not merely from personality differences [25].
Emotional Flooding and Biological Synchrony
Couples in conflict exhibit hormonal covariation: as one partner’s cortisol rises, the other’s tends to follow [26]. Emotional flooding, when both partners surpass their physiological threshold for reasoning, corresponds to a mutual cortisol spike. High physiological arousal correlates with defensive behavior, stonewalling, and criticism [38]. Without a deliberate pause, neither partner’s system resets, prolonging hostility.
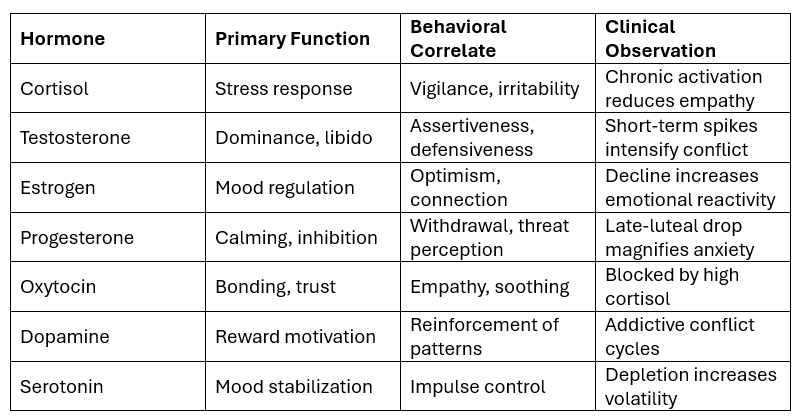
Table 1 presents the major hormones, behavioral correlates, and clinical implications relevant to couple conflict.
Biological Blocks to De-escalation and Intimacy
Cortisol–Oxytocin Antagonism
Cortisol and oxytocin are functional opposites. Cortisol activates defense; oxytocin promotes approach [27]. High cortisol reduces oxytocin receptor sensitivity, rendering affectionate acts ineffective. Over time, couples report feeling “numb” to kindness or touch. The relationship enters an emotional drought, a physiologic condition, not a lack of will.
Testosterone–Cortisol Cross-Talk
In men, cortisol and testosterone interact bidirectionally. Acute stress may boost testosterone, producing aggressive engagement, while chronic stress lowers it [12][29]. This results in a pattern where a man initially argues forcefully, then retreats. The partner perceives volatility or avoidance, unaware that endocrine exhaustion drives the switch. In women, cortisol suppresses estrogen and progesterone, decreasing libido and empathy [30]. Thus, chronic tension erodes both sexual desire and emotional bonding.
Dopamine, Reward, and the Addiction to Conflict
Conflict followed by reconciliation produces dopamine bursts [31]. These unpredictable rewards reinforce the very arguments partners wish to avoid. When peace feels dull, the brain subconsciously seeks stimulation through renewed disagreement. This pattern mirrors behavioral addiction [32]. Awareness of this neurochemical reinforcement can reframe volatile relationships as biologically conditioned loops rather than purely psychological dysfunction.
Serotonin and Regulation Failures
Low serotonin undermines patience and impulse control [19][33]. Minor irritations become major offenses. Restoring sleep, nutrition, and aerobic activity can elevate serotonin and reduce escalation frequency. SSRIs, by increasing serotonin availability, often stabilize relationships indirectly by reducing reactivity [34].
Clinical Implications and Applications
1. Psychoeducation and Biological Compassion
Educating couples about hormonal feedback normalizes reactivity. Reframing “You’re overreacting” as “Your cortisol is high and oxytocin is low” reduces shame [35]. Understanding PMDD or stress-induced withdrawal as physiological fosters empathy. Partners become collaborators in regulation rather than adversaries in blame.
2. Timing Conversations Around Hormonal Rhythms
For many women, the follicular phase offers emotional balance; for men, regulation improves with rest and low external stress [36]. Clinicians should guide couples to schedule sensitive discussions during physiologically stable periods. This respects biology’s rhythms rather than opposing them.
3. Restoring Cortisol–Oxytocin Balance
Joint breathing, affectionate nonsexual touch, laughter, and synchronized activities raise oxytocin and lower cortisol [37]. Deliberate breaks during arguments allow cortisol to metabolize [38]. When partners resume discussion post-calm, empathy and problem-solving improve dramatically.
4. Identifying Hormonal Disorders
Screening for PMDD, perimenopause, or stress-related hypogonadism clarifies whether mood instability stems from endocrine or relational causes [39][40]. Treating physiological contributors reduces misattributed blame and restores intimacy potential.
5. Biological Synchrony as a Therapeutic Target
Couples whose cortisol rhythms synchronize show higher satisfaction [9][41]. Therapists can cultivate synchrony through shared mindfulness and coordinated rituals. Over time, partners learn to sense misalignment and pause before escalation.
Figure 1 illustrates the interlocking hormonal feedback loops underlying escalation and repair:
Stress activation: perceived threat → HPA axis → cortisol surge.
Attachment suppression: cortisol ↑ → oxytocin ↓ → empathy loss.
Dominance and defense: testosterone ↑ (cortisol-moderated) → argument or withdrawal.
Reward reinforcement: dopamine ↑ during reconciliation → cycle repetition.
Chronic dysregulation: sustained imbalance → trust erosion and sexual disconnection.
Discussion
The evidence indicates that intimate conflict is a biological event as much as a psychological one. Each hormone contributes to a system of feedback loops that bias partners toward either approach or avoidance. Female physiology, characterized by monthly hormonal variability, frequently sustains activation longer, whereas male physiology favors rapid arousal and withdrawal. Together, these rhythms form a complementary but self-perpetuating pattern of pursuit and retreat [25][27].
Understanding these dynamics reframes relational dysfunction as biological misattunement. When one partner’s nervous system signals “connect” and the other’s signals “protect,” dialogue collapses. The resulting frustration is not moral failure but neuroendocrine incompatibility in that moment. Interventions that lower cortisol, restore oxytocin, and respect cyclic variability can therefore re-establish emotional safety more effectively than cognitive insight alone.
Limitations
While hormonal feedback models provide powerful explanatory value, they must be understood within an integrated biopsychosocial framework. Biological predispositions interact with early attachment experiences, trauma histories, cultural expectations, and communication styles. No hormone acts in isolation; contextual factors such as sleep, nutrition, and social support profoundly influence endocrine expression [3][6].
Another limitation concerns research methodology. Most hormone–behavior data derive from laboratory studies with limited ecological validity. Real-life couple interactions involve overlapping stressors, circadian rhythms, and external demands that are difficult to replicate experimentally. Additionally, female hormonal phases vary widely between individuals, complicating the interpretation of “average” effects [17][36]. Future work using real-time hormonal sampling, wearable sensors, and longitudinal tracking of couple synchrony will provide more precise insights into how biological rhythms shape intimacy and resilience.
Finally, while this paper emphasizes female cyclic contributions to conflict escalation, this focus should not be misconstrued as pathologizing female biology. Rather, it highlights the importance of understanding how endocrine fluctuations, predictable and natural, intersect with modern relational demands that ignore those rhythms. Recognition allows adaptation, not blame.
Coregulation in Couple Therapy
Coregulation refers to the mutual modulation of emotional and physiological states between partners through verbal and nonverbal cues. In couple therapy, it is the process by which two individuals influence one another’s arousal, affect, and physiological stability during interaction [42][43]. It is the interpersonal extension of self-regulation: where self-regulation involves internal modulation, coregulation occurs between people through eye contact, tone, touch, and presence [44].
Healthy relationships rely on partners who act as external regulators of one another’s nervous systems. When functioning well, each partner helps the other return to equilibrium after distress. In distressed relationships, partners instead trigger one another’s defensive or threat responses, creating cycles of mutual dysregulation [45][46].
Biological Basis
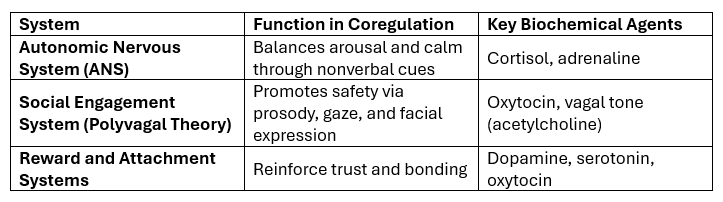
Coregulation is supported by overlapping autonomic, hormonal, and neural systems:
Partners’ nervous systems continuously “read” and respond to one another. When one partner experiences distress, the other’s calm and empathic cues can downregulate stress responses, lowering cortisol and sympathetic activation [47]. Conversely, harsh tone or criticism amplifies cortisol and adrenaline in both individuals [48].
This creates a bi-directional feedback loop: one partner’s calm can regulate both, while one partner’s arousal can dysregulate both [49].
Clinical Application
In therapy, coregulation is both a goal and a mechanism of change. The therapist initially models regulation by maintaining calm prosody, validating both partners, and pacing conversation to reduce arousal [50]. Over time, partners are coached to use co-regulatory behaviors directly, such as:
Gentle vocal tone and softened eye contact
Slow breathing and open posture
Validation (“I can see that was hard for you”)
Safe touch (when appropriate)
Therapists help couples notice when arousal exceeds tolerance and pause interaction, allowing physiological recovery before problem-solving resumes [51].
When partners reestablish a rhythm of mutual calming and safety cues, their oxytocin and serotonin levels increase, reinforcing trust and connection [52]. This is why interventions like synchronized breathing, affectionate touch, and emotionally attuned listening are biologically powerful—they literally alter the couple’s chemistry.
Coregulation vs. Codependence
Healthy coregulation is reciprocal and strengthens autonomy. It differs from codependence, where one partner overfunctions emotionally for the other. Coregulation supports self-regulation; codependence replaces it [53]. Therapists frame this distinction explicitly so that clients learn interdependence without loss of individuality.
Coregulation Failure
When couples chronically fail to coregulate, both partners’ HPA axes remain activated, sustaining high cortisol and suppressing oxytocin. Over time, this erodes empathy, attachment, and trust [54]. Partners synchronize around threat, not safety—creating a biological stalemate that sustains conflict and emotional distance [55].
The aim of therapy, therefore, is to restore biological synchrony around safety—a state where both nervous systems can downshift from defense to connection.
Conclusion
Intimate partnerships represent one of humanity’s most biologically demanding contexts. The same hormonal systems that evolved to ensure survival and reproduction, cortisol for vigilance, testosterone for competition, estrogen and progesterone for reproduction, oxytocin for bonding, now regulate the emotional microclimates of our daily relationships. When these systems operate harmoniously, they create empathy, desire, and trust. When misaligned, they generate cycles of conflict, withdrawal, and disconnection.
Understanding these feedback loops allows clinicians and couples alike to view conflict not as character failure but as physiological overload. The body, not just the mind, must calm for reconciliation to occur. Respecting hormonal timing, reducing stress arousal, and fostering oxytocin-rich connection provide an evidence-based roadmap for sustaining intimacy.
Ultimately, biological compassion, the recognition that our neuroendocrine architecture both binds and betrays us, may be the most powerful therapeutic insight of all. When partners learn to regulate physiology together, they rediscover that love is not merely an emotion but a coordinated biological rhythm.
References
[1] Taylor, S.E., Klein, L.C., Lewis, B.P., et al. 2000. Biobehavioral responses to stress in females: Tend-and-befriend, not fight-or-flight. Psychological Review, 107(3):411–429.
https://doi.org/10.1037/0033-295X.107.3.411
[2] Kiecolt-Glaser, J.K., Loving, T.J., Stowell, J.R., et al. 2005. Hostile marital interactions, proinflammatory cytokine production, and wound healing. Archives of General Psychiatry, 62(12):1377–1384.
https://doi.org/10.1001/archpsyc.62.12.1377
[3] Sapolsky, R.M. 2004. Why Zebras Don’t Get Ulcers. New York: Henry Holt & Co.
https://www.henryholt.com/books/9780805073690
[4] LeDoux, J.E. 2012. Rethinking the emotional brain. Neuron, 73(4):653–676.
https://doi.org/10.1016/j.neuron.2012.02.004
[5] Schoep, M.E., Nieboer, T.E., van der Zanden, M., Braat, D.D.M., Nap, A.W. 2019. Productivity loss due to menstruation-related symptoms: nationwide survey of 32,748 women. BMJ Open, 9:e026186.
https://bmjopen.bmj.com/content/9/6/e026186
[6] Archer, J. 2002. Sex differences in physically aggressive acts between heterosexual partners: A meta-analytic review. Aggression and Violent Behavior, 7(4):313–351.
https://doi.org/10.1016/S1359-1789(01)00061-1
[7] McEwen, B.S. 2007. Physiology and neurobiology of stress and adaptation: central role of the brain. Physiological Reviews, 87(3):873–904.
https://doi.org/10.1152/physrev.00041.2006
[8] Buchanan, T.W., & Lovallo, W.R. 2001. Enhanced memory for emotional material following stress-level cortisol treatment in humans. Psychoneuroendocrinology, 26(3):307–317.
https://doi.org/10.1016/S0306-4530(00)00062-0
[9] Laurent, H.K., Powers, S.I., & Granger, D.A. 2016. Cortisol synchrony and couple relationship functioning. Psychoneuroendocrinology, 63:119–128.
https://doi.org/10.1016/j.psyneuen.2015.09.022
[10] Mazur, A., & Booth, A. 1998. Testosterone and dominance in men. Behavioral and Brain Sciences, 21(3):353–397.
https://doi.org/10.1017/S0140525X98001228
[11] Carré, J.M., & Olmstead, N.A. 2015. Social neuroendocrinology of human aggression: Examining the role of competition and testosterone. Frontiers in Psychology, 6:132.
https://doi.org/10.3389/fpsyg.2015.00132
[12] Mehta, P.H., & Josephs, R.A. 2010. Testosterone and cortisol jointly regulate dominance: Evidence for a dual-hormone hypothesis. Hormones and Behavior, 58(5):898–906.
https://doi.org/10.1016/j.yhbeh.2010.08.020
[13] Gray, P.B., Kahlenberg, S.M., Barrett, E.S., Lipson, S.F., & Ellison, P.T. 2002. Marriage, fatherhood, and testosterone. Nature, 417(6890):801–802.
https://doi.org/10.1038/417801a
[14] Barth, C., Villringer, A., & Sacher, J. 2015. Current concepts of estrogen and progesterone action in the brain: regulation of mood, cognition, and neuroplasticity. Frontiers in Neuroendocrinology, 38:89–104.
https://doi.org/10.1016/j.yfrne.2015.02.004
[15] Freeman, E.W. 2013. Premenstrual syndrome and premenstrual dysphoric disorder: Definitions and diagnosis. Psychoneuroendocrinology, 38(6):1160–1164.
https://doi.org/10.1016/j.psyneuen.2012.11.013
[16] Yonkers, K.A., O'Brien, P.M.S., & Eriksson, E. 2008. Premenstrual syndrome. The Lancet, 371(9619):1200–1210.
https://doi.org/10.1016/S0140-6736(08)60527-9
[17] Romans, S.E., Clarkson, R., Einstein, G., Petrovic, M., & Stewart, D.E. 2012. Mood and the menstrual cycle: A review of prospective data studies. Journal of Affective Disorders, 142(1–3):4–13.
https://doi.org/10.1016/j.jad.2012.05.019
[18] Fisher, H.E., Aron, A., & Brown, L.L. 2006. Romantic love: A mammalian brain system for mate choice. Philosophical Transactions of the Royal Society B, 361(1476):2173–2186.
https://doi.org/10.1098/rstb.2006.1938
[19] Coccaro, E.F., Lee, R., & McCloskey, M.S. 2010. Serotonin and impulsive aggression. Annals of the New York Academy of Sciences, 1036:82–94.
https://doi.org/10.1196/annals.1330.006
[20] Halbreich, U., & Kahn, L.S. 2001. Role of estrogen in mood disorders. CNS Drugs, 15(10):797–817.
https://doi.org/10.2165/00023210-200115100-00003
[21] Carter, C.S. 2014. Oxytocin pathways and the evolution of human behavior. Annual Review of
Psychology, 65:17–39.
https://doi.org/10.1146/annurev-psych-010213-115110
[22] Ditzen, B., Schaer, M., Gabriel, B., Bodenmann, G., Ehlert, U., & Heinrichs, M. 2009. Intranasal oxytocin increases positive communication and reduces cortisol during couple conflict. Biological Psychiatry, 65(9):728–731.
https://doi.org/10.1016/j.biopsych.2008.10.011
[23] Bartz, J.A., et al. 2011. Oxytocin selectively improves empathic accuracy. Psychological Science, 21(10):1426–1428.
https://doi.org/10.1177/0956797610383439
[24] Pletzer, B., Kronbichler, M., Ladurner, G., & Kerschbaum, H.H. 2016. Cyclic changes in brain activation and connectivity across the menstrual cycle. Frontiers in Human Neuroscience, 10:613.
https://doi.org/10.3389/fnhum.2016.00613
[25] Gottman, J.M., & Levenson, R.W. 1999. Revisiting the divorce prediction study. Family Process, 38(2):179–193.
https://doi.org/10.1111/j.1545-5300.1999.00179.x
[26] Saxbe, D.E., Repetti, R.L., & Nishina, A. 2014. Couples’ cortisol covariation and marital satisfaction. Health Psychology, 33(11):1245–1253.
https://doi.org/10.1037/hea0000127
[27] Neumann, I.D. 2008. Brain oxytocin: A key regulator of emotional and social behaviors in both sexes. Frontiers in Neuroendocrinology, 29(3):267–295.
https://doi.org/10.1016/j.yfrne.2008.01.002
[28] Gunnar, M.R., & Quevedo, K.M. 2007. The neurobiology of stress and development. Annual Review of Psychology, 58:145–173.
https://doi.org/10.1146/annurev.psych.58.110405.085605
[29] Tilbrook, A.J., Turner, A.I., & Clarke, I.J. 2000. Stress and reproduction: central mechanisms and sex differences. Reviews of Reproduction, 5(2):105–113.
https://doi.org/10.1530/ror.0.0050105
[30] Chrousos, G.P. 2009. Stress and disorders of the stress system. Nature Reviews Endocrinology, 5(7):374–381.
https://doi.org/10.1038/nrendo.2009.106
[31] Volkow, N.D., Wang, G.-J., Fowler, J.S., & Tomasi, D. 2011. Dopamine reward pathways in addiction. Biological Psychiatry, 69(12):e145–e152.
https://doi.org/10.1016/j.biopsych.2010.11.014
[32] Goldstein, R.Z., & Volkow, N.D. 2011. Dysfunction of the prefrontal cortex in addiction: implications for self-control. Nature Reviews Neuroscience, 12(11):652–669.
https://doi.org/10.1038/nrn3119
[33] Steiner, M., Born, L., & Shapiro, C. 2003. Serotonin and premenstrual dysphoric disorder. Pharmacopsychiatry, 36(Suppl 3):S89–S95.
https://doi.org/10.1055/s-2003-45122
[34] Rapkin, A.J., & Lewis, E.I. 2013. Treatment of premenstrual dysphoric disorder. Journal of Clinical Psychiatry, 74(6):e14–e21.
https://doi.org/10.4088/JCP.12002co1c
[35] Johnson, S.M. 2019. Attachment Theory in Practice: Emotionally Focused Therapy (EFT) for Individuals, Couples, and Families. New York: Guilford Press.
https://www.guilford.com/books/Attachment-Theory-in-Practice/Susan-M-Johnson/9781462538249
[36] Direkvand-Moghadam, A., Sayehmiri, K., Delpisheh, A., & Kaikhavani, S. 2014. Epidemiology of PMS: Systematic review and meta-analysis. Journal of Clinical and Diagnostic Research, 8(4):106–109.
https://doi.org/10.7860/JCDR/2014/8024.4269
[37] Schneiderman, I., Zagoory-Sharon, O., Leckman, J.F., & Feldman, R. 2012. Oxytocin and cortisol in romantic attachment: Associations with relationship stress. Psychoneuroendocrinology, 37(7):1277–1285.
URL: https://doi.org/10.1016/j.psyneuen.2011.12.011
[38] Gottman, J.M. 2011. The Science of Trust: Emotional Attunement for Couples. New York: W.W. Norton & Company.
https://wwnorton.com/books/9780393705959
[39] Epperson, C.N., Steiner, M., & Hartlage, S.A. 2012. Premenstrual dysphoric disorder: Evidence for a new category for DSM-5. American Journal of Psychiatry, 169(5):465–475. https://doi.org/10.1176/appi.ajp.2012.11081302
[40] Khera, M., Bhattacharya, R.K., Blick, G., et al. 2016. Testosterone deficiency in men: Pathophysiology and treatment. Mayo Clinic Proceedings, 91(7):881–896.
https://doi.org/10.1016/j.mayocp.2016.03.018
[41] Saxbe, D.E., & Repetti, R.L. 2010. For better or worse? Coregulation of couples’ cortisol levels and mood states. Journal of Personality and Social Psychology, 98(1):92–103. https://doi.org/10.1037/a0016959
[42] Schore, A.N. (2012). The Science of the Art of Psychotherapy. New York: W.W. Norton.
https://wwnorton.com/books/9780393706642
[43] Porges, S.W. (2011). The Polyvagal Theory: Neurophysiological Foundations of Emotions, Attachment, Communication, and Self-Regulation. New York: W.W. Norton.
https://wwnorton.com/books/9780393707007
[44] Coan, J.A., & Maresh, E.L. (2014). Social baseline theory and the social regulation of emotion. In M. Mikulincer & P.R. Shaver (Eds.), Mechanisms of Social Connection (pp. 79–88). Washington, DC: American Psychological Association.
https://doi.org/10.1037/14250-005
[45] Gottman, J.M. (2011). The Science of Trust: Emotional Attunement for Couples. New York: W.W. Norton.
https://wwnorton.com/books/9780393705959
[46] Johnson, S.M. (2019). Attachment Theory in Practice: Emotionally Focused Therapy (EFT) with Individuals, Couples, and Families. New York: Guilford Press.
https://www.guilford.com/books/Attachment-Theory-in-Practice/Susan-M-Johnson/9781462538249
[47] Coan, J.A., Schaefer, H.S., & Davidson, R.J. (2006). Lending a hand: Social regulation of the neural response to threat. Psychological Science, 17(12), 1032–1039.
https://doi.org/10.1111/j.1467-9280.2006.01832.x
[48] Laurent, H.K., & Powers, S.I. (2007). Emotion regulation in emerging adult couples: Temperament, attachment, and HPA response to conflict. Biological Psychology, 76(1–2), 61–71.
https://doi.org/10.1016/j.biopsycho.2007.06.002
[49] Reed, R.G., Barnard, K., & Butler, E.A. (2015). Distinguishing emotional coregulation from codysregulation: A process model of dyadic emotional dynamics. Emotion Review, 7(1), 14–25.
https://doi.org/10.1177/1754073914544474
[50] Sbarra, D.A., & Hazan, C. (2008). Coregulation, dysregulation, self-regulation: An integrative analysis and empirical agenda for attachment theory. Emotion, 8(4), 505–517.
https://doi.org/10.1037/a0012764
[51] Gottman, J.M., & Silver, N. (2015). The Seven Principles for Making Marriage Work (2nd ed.). New York: Harmony Books.
https://www.penguinrandomhouse.com/books/189673/the-seven-principles-for-making-marriage-work-by-john-gottman-phd-and-nan-silver/
[52] Ditzen, B., et al. (2009). Intranasal oxytocin increases positive communication and reduces cortisol during couple conflict. Biological Psychiatry, 65(9), 728–731.
https://doi.org/10.1016/j.biopsych.2008.10.011
[53] Tatkin, S. (2012). Wired for Love: How Understanding Your Partner’s Brain and Attachment Style Can Help You Defuse Conflict and Build a Secure Relationship. Oakland, CA: New Harbinger Publications.
https://www.newharbinger.com/9781608820580/wired-for-love/
[54] Schneiderman, I., Zagoory-Sharon, O., Leckman, J.F., & Feldman, R. (2012). Oxytocin and cortisol in romantic attachment: Biological correlates of relationship functioning. Psychoneuroendocrinology, 37(7), 1277–1285.
https://doi.org/10.1016/j.psyneuen.2011.12.011
[55] Reed, R.G., Randall, A.K., Post, J.H., & Butler, E.A. (2013). Partner influence and coregulation of physiological stress in couples. Journal of Family Psychology, 27(4), 521–530.
https://doi.org/10.1037/a0033366