The GRID Charting Model in Outpatient Psychotherapy Documentation
Cover Memorandum
Purpose
This Memorandum is submitted to inform health plans, regulators, and utilization management entities about the evolution of psychotherapy documentation standards and to clarify why The GRID represents a fourth-generation documentation system for outpatient psychotherapy. This model is well-suited as framework for a hybrid use of AI to ensure charting is useful for multiple real word clinical, ethical, legal, contractual, business and practice management purposes. The GRID provides a learning while you chart experience providing feedback while chart to ensure the providers is creating a reliable, valid and useful record.
Many payers recommend or expect “SMART charting” as a proxy for documentation quality. The attached paper demonstrates that:
SMART charting reflects a third-generation documentation paradigm, developed for institutional and team-based care.
Outpatient psychotherapy presents fundamentally different clinical, ethical, and regulatory requirements.
The GRID captures the core intent of SMART charting inherently and more reliably, while also addressing privacy protection, audit defensibility, clinician burden, and workforce sustainability.
This cover memo highlights payer-specific relevance to assist reviewers in situating the paper within their regulatory and operational context.
Across Medicare, Medicaid, OHP, and commercial plans, the core documentation need is the same: reliable, interpretable, defensible outpatient psychotherapy records.
The GRID:
captures SMART attributes inherently,
reduces privacy and audit risk,
lowers administrative burden,
and supports stable provider networks.
Summary
SMART charting is understandable as a legacy standard, especially for organizations trained to expect goal language and session narrative as a proxy for quality and accountability. However, outpatient psychotherapy documentation must serve multiple purposes beyond treatment planning, including privacy protection, audit defensibility, legal risk management, and quality review (APA, 2007; CMS, 2014; King, 2014; MRI, 2025).
The GRID captures SMART dimensions inherently through structured clinical representation rather than narration and prose. This yields a record that is more reliable, more precise, more comprehensive, more valid for outpatient psychotherapy documentation realities, and more defensible under audit, while also supporting measurement-based care and minimum-necessary privacy principles (HHS, 2017; Lewis et al., 2019; Shanafelt et al., 2016).
Historical Evolution of Psychotherapy Documentation Systems
Before comparing SMART Charting and The GRID directly, it is necessary to situate both approaches within the broader historical evolution of psychotherapy documentation. Documentation systems have developed in distinct generations, each responding to the clinical, regulatory, and ethical limitations of the prior era. Understanding this evolution clarifies why SMART charting emerged, why it became dominant, and why a fourth-generation system is now necessary for outpatient psychotherapy.
Generation 1: Paper Records and SOAP Notes (Mid-20th Century – 1990s)
In the early decades of outpatient psychotherapy, documentation was entirely paper-based. Therapists maintained handwritten notes in physical files stored in offices and secured cabinets (Blueprint, 2025). The style and content of notes were largely unstandardized until the mid-20th century, when efforts began to introduce more structure. One landmark was the development of the SOAP note format (Subjective, Objective, Assessment, Plan) by Dr. Lawrence Weed in the 1950s (Yung Sidekick, 2024). SOAP notes brought a logical order to clinical entries, ensuring key information (the client’s subjective report, the therapist’s observations, clinical assessment, and the treatment plan) was captured consistently (Yung Sidekick, 2024). Variations like DAP (Data, Assessment, Plan) and BIRP notes also emerged, but all were concise narrative tools guided by clinical reasoning (Yung Sidekick, 2024).
Clinical and Ethical Dimensions: In this paper era, privacy and confidentiality were central and comparatively straightforward to maintain. Records were physical and usually accessible only to the treating clinician (Blueprint, 2025). Therapists could limit written details to protect sensitive patient disclosures, and many kept separate “psychotherapy notes” (process notes) intended for their own use. Freud’s practice is often cited historically to illustrate early awareness that excessive note-taking can disrupt the therapeutic process and rapport (Yung Sidekick, 2024). Notes were commonly written after sessions, preserving the immediacy of the therapeutic alliance.
However, outcome tracking was informal. Progress was noted in qualitative terms, and systematic outcome measurement was uncommon. Audit defensibility depended largely on individual practice habits; third-party audits of outpatient psychotherapy were less routine than they later became. Documentation burden remained relatively low.
Regulatory Context: The landscape shifted with the emergence of federal privacy standards. HIPAA’s Privacy Rule recognized psychotherapy notes as especially sensitive and provided distinct protections for them relative to other parts of the record (U.S. Department of Health & Human Services, 2017). Over time, the principle that psychotherapy depends on confidentiality remained a defining ethical and legal norm guiding documentation practices in outpatient psychotherapy (Mentor Research Institute, 2023).
Generation 2: Electronic Health Records and Traditional Note Formats (2000s)
The 2000s brought widespread digitization. Electronic Health Records (EHRs) promised improved efficiency, legibility, and integration. Adoption accelerated with national policy and incentives, even though many independent behavioral health clinicians did not directly benefit from incentive programs (Blueprint, 2025). Nevertheless, payer requirements and administrative modernization gradually made EHR use commonplace in outpatient mental health settings (Blueprint, 2025).
Clinical Impact: EHRs improved information accessibility and, in some settings, care coordination and safety alerts (Blueprint, 2025). They also enabled the integration of symptom scales and standardized measures into workflow—at least in theory. At the same time, many EHRs were designed for general medical workflows and were not well adapted to psychotherapy, producing usability problems and workflow friction (Blueprint, 2025). This contributed to therapists completing documentation after hours and experiencing increased administrative burden.
Privacy and Security: Digital records amplified confidentiality concerns. While electronic systems can be secured, they also introduced new risks: expanded access pathways, vendor involvement, and cybersecurity vulnerability (Documentation Wizard, 2024). The combination of digital storage and evolving “open notes” norms increased the need to carefully distinguish what belongs in the designated record set versus what should remain private psychotherapy notes (U.S. Department of Health & Human Services, 2017).
Audit and Compliance: EHRs increased standardization, but they also introduced copy-paste and “cloned note” risks. Regulators and auditors increasingly scrutinized repetitious or boilerplate language as a sign that notes may not reflect individualized clinical work (ICD10monitor, 2025). This became a major compliance driver and set the stage for the next phase: stronger payer pressure for “goal-driven” documentation.
Generation 3: SMART Charting (2010s)
By the 2010s, managed care expectations, institutional quality frameworks, and administrative standardization converged into a new documentation paradigm: SMART charting—treatment plans and progress notes organized around goals that are Specific, Measurable, Achievable/Attainable, Relevant, and Time-bound (Mentor Research Institute, 2023). SMART’s origin is managerial rather than clinical, and its migration into psychotherapy documentation was driven primarily by operational and payer imperatives rather than evidence that SMART documentation improves outpatient psychotherapy outcomes (Mentor Research Institute, 2023).
Clinical Practice Implications: SMART charting can impose a linear and quantifiable logic on psychotherapy that does not always fit outpatient clinical realities. Reviews and commentary summarized by Mentor Research Institute argue there is no empirical evidence that treatment plans and progress note structures required by external interests improve outcomes, patient satisfaction, or quality in outpatient psychotherapy (Mentor Research Institute, 2023). SMART also tends to rely on prose-based inference: “specificity” and “measurement” often become narrative exercises rather than structured clinical representations.
Ethical and Privacy Issues: Heavy documentation demands can produce “chilling effects,” including pressure to record sensitive personal details primarily to satisfy external reviewers, increasing privacy exposure and potentially impairing client openness (Independent Mental Health Practices Alliance & Mentor Research Institute, 2021; Mentor Research Institute, 2023). When documentation functions as an administrative artifact more than a clinical tool, it can distort sessions into data-gathering and justification exercises (Mentor Research Institute, 2023).
Administrative Burden: Generation 3 often increased documentation time and complexity. Clinics and systems frequently implemented chart-audit checklists, compliance scoring, and extensive treatment-plan requirements, intensifying workload and burnout risk (Eleos Health, 2020; Mentor Research Institute, 2023).
Generation 4: The GRID (2020s)
The modern response to Generation 2–3 burdens has been a shift toward documentation systems that maintain defensibility while reducing narrative inflation and protecting confidentiality. The GRID is presented as a structured, longitudinal framework designed for outpatient psychotherapy documentation, organized as a vertical-category/horizontal-session matrix that supports charting-by-exception, longitudinal comparability, and internal compliance logic (Mentor Research Institute, 2022; Blueprint, 2025).
Purpose and Philosophy: The GRID approach positions psychotherapy documentation as simultaneously clinical, ethical, and audit-aware, but not dependent on narrative volume. It makes requirements visible, supports minimum-necessary documentation, and aims to preserve the therapeutic process while still meeting payer and regulatory needs (Mentor Research Institute, 2022; Mentor Research Institute, 2023).
Audit Defensibility and Efficiency: The GRID is described as enabling “audit-assurance” documentation through structured fields, internal completeness checks, and defensibility controls (Mentor Research Institute, 2022). The concept is to decouple quality/compliance from sheer documentation volume: completeness is achieved through structure rather than prose (Mentor Research Institute, 2022).
Privacy and Alliance: A core ethical claim is that the GRID helps clinicians document what is necessary without capturing excessive sensitive narrative content, supporting HIPAA’s minimum-necessary principle and maintaining client trust (U.S. Department of Health & Human Services, 2017; Mentor Research Institute, 2023).
AI is Not Viable as a “Fifth Generation” Replacement for Psychotherapy Documentation (Late 2010s–2025)
AI is increasingly marketed as a remedy for documentation burden, including tools that transcribe or summarize psychotherapy sessions and draft progress notes (Documentation Wizard, 2024; Blueprint, 2025). While AI-assisted drafting may offer time savings, the proposition that AI is a viable stand-alone documentation method in outpatient psychotherapy faces major barriers across clinical, ethical, and regulatory domains.
Accuracy and Clinical Judgment: AI systems can generate plausible text that is incomplete, misleading, or factually incorrect (Documentation Wizard, 2024). In psychotherapy documentation, even small inaccuracies can be clinically and legally significant. AI-generated notes can also drift toward generic, boilerplate phrasing, creating the same audit vulnerability previously associated with cloned notes and copy-forward charting (ICD10monitor, 2025).
Privacy, Consent, and Trust: AI documentation workflows often require recording or transmitting highly sensitive information to third-party services. Even when vendors claim HIPAA compliance, the practical risks of data exposure, secondary use, and client mistrust remain substantial (Documentation Wizard, 2024). Ethical best practice trends increasingly emphasize transparency when technology materially changes how documentation is produced, especially when session recordings are involved (American Counseling Association, 2024; American Psychological Association, 2025).
Regulatory and Audit Defensibility: As of late 2025, professional guidance emphasizes that clinicians remain fully responsible for the content of the clinical record when AI tools are used; AI does not substitute for clinician authorship, judgment, or accountability (American Psychological Association, 2025). Auditors’ longstanding concerns about non-individualized documentation extend naturally to AI-generated text that appears templated or inconsistent with the clinician’s documented reasoning (ICD10monitor, 2025). In practical terms, AI may assist, but it does not remove the clinician’s duty to ensure that documentation accurately represents the clinical encounter and supports medical necessity.
Bottom line: AI may become an adjunct tool under strict human oversight, but it is not viable as an autonomous documentation “generation” for outpatient psychotherapy under current ethical expectations and audit realities (American Psychological Association, 2025; ICD10monitor, 2025; Documentation Wizard, 2024).
GRID vs. SMART Charting in Outpatient Psychotherapy Documentation
Introduction
Effective documentation in psychotherapy must balance clinical utility, compliance, and confidentiality. Two contrasting approaches are The GRID documentation system and SMART Charting. The GRID is a modern, adaptable charting platform designed for outpatient therapy, emphasizing efficient, audit-proof notes aligned with therapeutic goals. In contrast, SMART Charting (based on setting Specific, Measurable, Achievable/Attainable, Relevant, Time-bound goals) originated in highly structured inpatient and residential settings.
Many health plans recommend or require “SMART charting,” typically meaning that documentation reflects Specific, Measurable, Achievable/Attainable, Relevant, and Time-bound goals and progress. SMART is widely familiar and administratively convenient, but it was developed as a management framework and later became embedded in behavioral health documentation expectations through institutional and payer processes rather than through evidence demonstrating superiority in outpatient psychotherapy outcomes (Doran, 1981; Mentor Research Institute [MRI], n.d.).
Outpatient psychotherapy documentation has to accomplish more than “treatment planning.” Notes must support multiple legitimate purposes, often simultaneously: clinical continuity, ethical obligations, privacy protections, audit defensibility, billing support, supervision/quality review, legal/regulatory response, and risk management (American Psychological Association [APA], 2007; Centers for Medicare & Medicaid Services [CMS], 2014; King, 2014; MRI, n.d.). When a plan focuses primarily on SMART goal prose, it may inadvertently incentivize documentation that is less reliable, less precise, and more privacy-risky than necessary for outpatient care.
The GRID is positioned as a structured outpatient documentation system that captures the functional intent of SMART (clarity, measurement, feasibility, relevance, and time anchoring), but does so in a more comprehensive, precise, reliable, valid, and defensible manner—especially because it relies on structured categories and options rather than interpretive prose (MRI, n.d.). In short: SMART aims to discipline language; The GRID replaces ambiguous language with structure where structure is superior for outpatient documentation.
This paper explains:
why outpatient documentation needs differ from inpatient/residential documentation needs;
the limits of SMART charting in outpatient psychotherapy;
the other purposes that outpatient psychotherapy notes must serve;
how The GRID captures SMART dimensions inherently—more reliably—using the GRID → SMART Crosswalk Table (Correct S.M.A.R.T. Definitions); and
why audit protection, chart migration support, and compliance scoring materially change payer risk and provider network stability.
Detailed Descriptions (what each system is)
What is SMART Charting?
SMART Charting refers to a documentation approach centered on highly structured treatment planning and progress notes, often organized around SMART goals (Specific, Measurable, Achievable, Relevant, Time-bound). This method gained prominence in managed care and institutional settings as a means to standardize records and hold providers accountable to clear objectives. In inpatient and residential programs, such structure can be beneficial: it produces uniform plans that multiple staff can follow and that external reviewers (insurers, auditors) find easy to evaluate.
However, experts caution that SMART Charting is fundamentally a business and management tool, not a clinical technique to enhance therapy outcomes. In practice, SMART Charting’s emphasis on documentation metrics encourages supervisors and payers to focus on whether a therapist’s notes “check the right boxes” rather than on genuine patient progress. Over time, what began as a way to hold clinicians accountable can morph into holding patients accountable to predetermined benchmarks in their notes. This can distort the therapeutic process—for instance, therapists may feel pressured to interrogate clients for detailed symptoms and psychosocial histories solely to satisfy documentation demands, even when such detail is clinically irrelevant or intrusive.
In summary, SMART Charting’s structured, one-size-fits-all documentation was developed for environments with shift-based teams and rigorous oversight, not for the one-on-one, flexible nature of outpatient therapy. It prioritizes consistency and external review criteria over individualized clinical narrative.
What is The GRID?
The GRID is a documentation framework and software platform created to optimize outpatient psychotherapy records. It was designed to streamline note-taking, protect patient privacy, support outcome-focused care, and ensure audit compliance without imposing an inpatient-style burden on clinicians. It uses an adaptable-template approach: structure and prompts for required elements while allowing customization to different clinical styles and patient needs. It is explicitly described as not a simplistic “cookie cutter” template—providing unified documentation structure while maintaining clinician individuality through editable dropdowns, optional narrative fields, customizable intervention lists, and configurable practice guidelines.
From an operational standpoint, the GRID is described as a vertical-category, horizontal-session matrix where each psychotherapy session is a column and each documentation category is a row. The system emphasizes charting by exception (document what meaningfully changed) and supports longitudinal comparability across sessions.
From a payer/audit perspective, the GRID is positioned as all-in-one, audit-assurance documentation for psychotherapy, designed to meet psychotherapy CPT requirements, E/M psychotherapy add-on codes, and contextual Z-code documentation, with strong governance controls, role-based access, and automated internal compliance scoring using structured logic (not AI). It includes immutable versioning, addendum-only edits after signing, and full audit logs for defensibility.
It is also presented as an efficiency platform: “turns a 10-minute psychotherapy note into… as little as 30 seconds,” by eliminating narrative redundancy via exception-based structure, reusable clinical options, and side-by-side charting.
Outpatient vs. Inpatient/Residential Documentation Needs
Inpatient/residential settings: documentation is a team handoff tool
In inpatient and residential behavioral health, documentation is essential for multidisciplinary coordination, shift-to-shift handoffs, and standardization under accreditation and facility policy. In these environments, highly structured treatment plans and extensive documentation can be rational because the record must communicate clinical status and plan across multiple professionals who may not know the patient directly. Hospitals and agencies often strive for uniform treatment plans with clearly defined problems, goals, and interventions in every chart to ease the task of record reviewers such as accreditation auditors.
In inpatient/residential care, a well-detailed plan is essential: new providers coming on duty may have never met the patient and must rely on the chart for guidance.
Outpatient psychotherapy: documentation is not a shift-handoff tool
Outpatient psychotherapy is typically characterized by:
one clinician,
episodic encounters,
continuity by relationship rather than chart handoff, and
far greater likelihood that notes will be reviewed by external parties (payers, auditors, courts) rather than by an internal team.
In outpatient psychotherapy, imposing inpatient-style documentation standards creates burdens without demonstrated clinical benefit, and it increases privacy and legal risk by encouraging narrative overproduction (King, 2014; MRI, n.d.). This setting difference is pivotal: SMART charting often reflects the documentation logic of institutional environments, whereas outpatient therapy requires a record that is simultaneously defensible and minimal-necessary.
The Limits of SMART Charting in Outpatient Psychotherapy
SMART is attractive because it seems to produce clarity. However, in outpatient psychotherapy, SMART charting often produces apparent clarity through prose rather than operational clarity through structured representation. Common outpatient problems with SMART-driven documentation include:
Narrative dependence and interpretive variability
Two competent clinicians can write “specific” and “measurable” goals that are not comparable or consistently interpretable. This is a reliability problem (King, 2014).Incentives toward over-documentation
When “specificity” is interpreted as “include more detail,” notes can drift toward documenting sensitive content unnecessarily, increasing risk if records are requested, audited, or litigated (APA, 2007; HHS, 2017).Conflation of accountability language with clinical truth
SMART can push clinicians toward treating goals as contractual deliverables rather than clinical hypotheses responsive to complexity and nonlinear change (MRI, n.d.).Workflow and burnout burden
Documentation burden is associated with clinician burnout and reduced professional satisfaction; systems that increase clerical load without clinical return create systemic harm (Shanafelt et al., 2016).
These limitations are not an argument that “goals” or “measurement” are unimportant. They are an argument that SMART as a prose-centered charting standard is a weak instrument for outpatient psychotherapy documentation.
The Multiple Purposes of Outpatient Psychotherapy Chart Notes
Health plans often focus on documentation for authorization and payment integrity. But outpatient psychotherapy documentation must support a broader set of legitimate purposes recognized in professional guidance and compliance standards:
Clinical care and continuity (within outpatient practice)
Notes support the clinician’s longitudinal understanding of presenting problems, clinical formulation, interventions used, response to treatment, and decision-making over time (APA, 2007; King, 2014).Patient protection and ethical accountability
Records can protect patients by documenting informed consent, risk assessment and response, appropriate referrals, and clinically indicated safety actions (APA, 2007; CMS, 2014).Privacy protection and minimum-necessary compliance
Outpatient psychotherapy requires heightened attention to confidentiality and “minimum necessary” principles, including the distinction between psychotherapy notes and the designated record set (45 C.F.R. § 164.501; HHS, 2017). Documentation that is too detailed can be clinically counterproductive and legally hazardous.Billing support and audit defensibility
Payers and auditors require that records support claims and “fully disclose the extent of services” necessary to validate billing and medical necessity (CMS, 2014). Importantly, “defensible” does not require “maximal narrative”; it requires clear linkage between diagnosis/need, service delivered, and progress/plan.Legal and regulatory response
Records are used in audits, investigations, licensing inquiries, subpoenas, and malpractice contexts. Notes must be intelligible to third parties and defensible without requiring inference about what the clinician “meant” (King, 2014).Quality improvement and supervision
Structured documentation supports peer review and quality assurance by making core clinical elements comparable across time and (when applicable) across clinicians (APA, 2007).
A key implication for payers: outpatient documentation systems should be evaluated not only by whether they contain SMART goal language, but by whether they reliably support these multiple purposes with minimal privacy exposure.
The GRID as a Structured Outpatient Psychotherapy Record System
The GRID is presented as a structured documentation architecture that reduces reliance on prose interpretation by using consistent clinical categories, constrained options, and longitudinal comparability (MRI, n.d.). This directly addresses the most common weaknesses of SMART charting in outpatient settings: variability, narrative inflation, and ambiguity under audit.
This is not “less documentation.” It is more disciplined documentation—more precise, more comparable, and more defensible because it is structured.
How The GRID addresses six essential documentation dimensions (outpatient-relevant)
Alignment with clinical and therapeutic purposes
A core principle of The GRID is that documentation should serve the clinical and therapeutic aims of treatment, not impede them. Traditional SMART-style charting often dictates the content of notes to satisfy administrators or insurers, which can divert therapy sessions into data-gathering exercises and cause cognitive dissonance for clinicians. In contrast, The GRID focuses on capturing what is clinically relevant: guiding therapists to document the minimum necessary information needed to justify treatment and support the patient’s goals, omitting unnecessary narrative or private therapeutic details from progress notes. This aligns with recommendations that outpatient therapy records be lean and focused to protect privacy if records are sought by insurers or third parties.Clinical nuance and clinician autonomy
The GRID is not a rigid template that forces every therapist to sound the same. It includes editable dropdowns, optional narrative fields, and customizable intervention lists to maintain clinician individuality while still creating unified documentation structure.Audit defensibility and integrity controls
The GRID is described as exceeding regulatory, ethical, and payer documentation standards via audit logs, scoring of notes against standards, and alignment with HIPAA and CMS rules. Each note is evaluated using structured logic (not AI). Notes are protected with immutable versioning and addendum-only corrections after signing, and every change is logged—design features that increase defensibility in payer review, compliance audits, or litigation.Privacy protection as a structural feature
The HIPAA Privacy Rule defines psychotherapy notes narrowly and distinguishes them from medical record elements required for treatment and payment (45 C.F.R. § 164.501). HHS guidance emphasizes that psychotherapy notes do not include diagnosis, functional status, treatment plan, symptoms, prognosis, and progress—those belong in the standard record. The GRID’s structured approach supports cleaner separation between what belongs in the designated record set and what should remain outside it to protect privacy and the therapeutic process.Measurement-based care compatibility
The GRID architecture supports PROMs and longitudinal tracking (e.g., PROM deltas and checkbox selections showing measurable change), linking interventions to goals and progress while minimizing narrative padding.Workflow burden reduction and network stability
Documentation burden is not just a clinician complaint; it is a payer stability issue. Burnout, network churn, and reduced access correlate with administrative burden and clerical load. A structured record architecture can reduce variability and time cost while improving defensibility—aligning payer integrity goals with clinician sustainability goals.
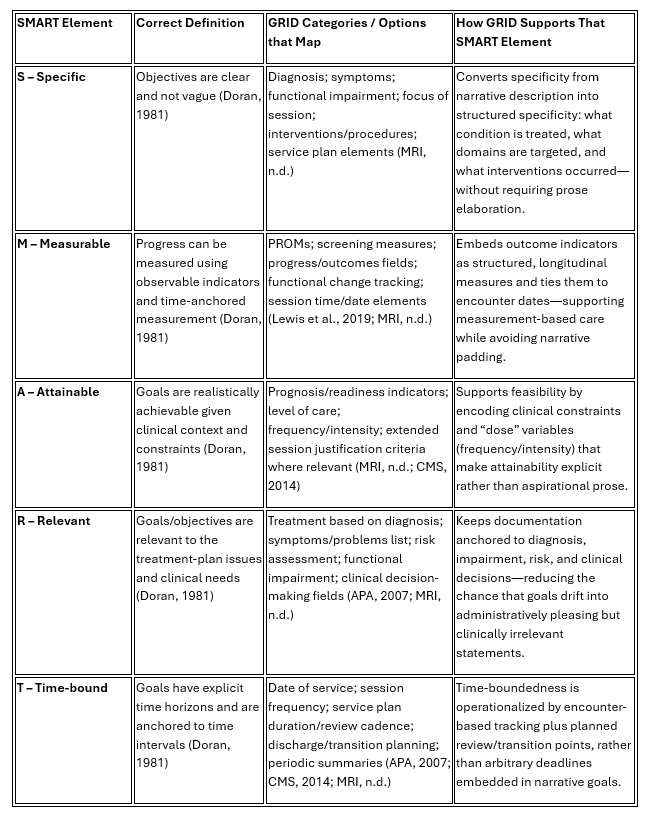
SMART and GRID Crosswalk Table
Following is a mapping of GRID categories SMART Charting categories and options. SMART categories as mapped to Specific, Measurable, Attainable, Relevant, Time-bound.
Table 1 SMART and GRID Crosswalk Table
Why this Crosswalk Matters
A payer’s legitimate objective is not “SMART prose.” It is a record that reliably shows:
what condition/impairment is being treated,
what service was delivered,
why that service remains medically reasonable and necessary, and
what changed or what problems were managed over time (managed deterioration).
CMS guidance emphasizes that records must support the claim and substantiate the billed level of care, and that insufficient documentation can justify denial (CMS, 2014). The GRID’s structured approach supports this goal more directly than narrative SMART charting because it reduces interpretive ambiguity and omission risk.
Privacy and the Psychotherapy Notes distinction: A Structural Advantage (not just a policy)
The HIPAA Privacy Rule defines psychotherapy notes narrowly and distinguishes them from the broader medical record elements needed for treatment and payment (45 C.F.R. § 164.501). HHS guidance emphasizes that psychotherapy notes do not include items such as diagnosis, functional status, treatment plan, symptoms, prognosis, and progress—those belong to the standard medical record (HHS, 2017).
For outpatient psychotherapy, this regulatory distinction matters because over-documentation can blur boundaries and increase exposure. A structured system like The GRID supports a cleaner separation between:
what must be in medical record set,
the designated record set for payment and continuity, and
what should remain outside it to protect privacy and the therapeutic process.
The GRID’s Audit-Assurance Architecture
The GRID is described as integrating: immutable versioning, addendum-only edits after signing, full audit logs for every data change, and structured categories that fulfill payer-required elements—creating a defensible record that withstands payer review, malpractice scrutiny, and compliance audits. It also includes automated internal compliance scoring (without AI) aligned to ethical standards, legal requirements, Medicare psychotherapy rules, Medicaid/OHP standards, CPT time/service specifications, and risk-assessment documentation expectations. Clinicians receive real-time feedback, supporting consistent compliance and reducing audit exposure.
It is also engineered for scale (solo providers through multi-clinic networks) with governance controls: role-based PHI access, “data walls” between clinics, and controlled cross-clinic visibility for authorized leadership—framing audit integrity as an organizational system, not just an individual clinician task.
Summary for Commercial Health Plans
Why the GRID Reduces Administrative Cost and Audit Friction Beyond SMART Charting
Many payers recommend or expect “SMART charting” as a proxy for documentation quality. This paper demonstrates that:
SMART charting reflects a third-generation documentation paradigm, developed for cost control, and institutional and team-based care;
Outpatient psychotherapy presents fundamentally different clinical, ethical, and regulatory requirements; and
The GRID captures the core intent of SMART charting inherently and more reliably, while also addressing privacy protection, audit defensibility, clinician burden, and workforce sustainability.
This cover memo highlights payer-specific relevance to assist reviewers in situating the paper within their regulatory and operational context.
Medicare (CMS / Medicare Administrative Contractors)
Medicare psychotherapy documentation requirements do not mandate SMART goals. CMS requires documentation that demonstrates:
medical reasonableness and necessity,
accurate CPT coding and time,
individualized clinical judgment,
patient response and rationale for continued care,
and audit-defensible records.
The GRID aligns directly with Medicare standards by structurally documenting diagnosis, impairment, service delivery, time, and response to treatment—without relying on narrative SMART goal prose that CMS does not require.
For Medicare reviewers, GRID-based records:
reduce interpretive ambiguity,
improve inter-rater reliability,
support post-payment audit review,
and align with HIPAA minimum-necessary principles.
The attached paper explains why acceptance of GRID-based documentation satisfies Medicare expectations while reducing administrative friction.
Medicaid (State Plans and Managed Care Organizations)
State Medicaid programs must balance program integrity with access to care and provider sustainability. SMART charting entered Medicaid largely through community mental health and residential standards and has since been applied broadly to outpatient psychotherapy.
In outpatient settings, SMART-driven documentation has contributed to:
excessive narrative documentation,
increased privacy exposure for vulnerable populations,
provider burnout and network churn,
and audit disputes driven by interpretive differences.
The GRID supports Medicaid objectives by:
standardizing core clinical elements,
improving audit consistency,
supporting ethical migration of legacy records,
and reducing unnecessary documentation burden.
The attached paper details how fourth-generation documentation improves both compliance and access, advancing Medicaid’s dual mandate.
Oregon Health Plan (OHP / Coordinated Care Organizations)
OHP and CCOs operate within a policy environment emphasizing:
value-based care,
health equity,
trauma-informed systems,
administrative simplification,
and workforce stability.
SMART charting conventions—borrowed from institutional models—often conflict with these goals in outpatient psychotherapy by increasing administrative burden and re-exposing sensitive content without clinical benefit.
The GRID aligns with OHP priorities by:
operationalizing minimum-necessary, trauma-informed documentation,
supporting measurement-based care without narrative inflation,
reducing audit-related fear and attrition among providers,
and integrating consultation and audit-protection infrastructure.
The attached paper situates the GRID within OHP’s policy framework and explains why it better supports equitable, sustainable outpatient care.
Commercial Health Plans
Commercial plans prioritize:
utilization management efficiency,
predictable audit outcomes,
network adequacy and retention,
and administrative cost control.
SMART charting has functioned as a heuristic for accountability but often results in:
inconsistent narrative records,
higher appeal and grievance rates,
and increased provider dissatisfaction.
The GRID benefits commercial plans by:
delivering standardized, interpretable documentation,
reducing reviewer subjectivity,
shortening audit cycles,
lowering dispute rates,
and improving provider retention.
The attached paper explains how GRID-based documentation answers the operational questions commercial reviewers actually ask: What was done, why was it necessary, and did it work?
Closing Statement
Across Medicare, Medicaid, OHP, and commercial plans, the core documentation need is the same: reliable, interpretable, defensible outpatient psychotherapy records.
The GRID:
captures SMART attributes inherently,
reduces privacy and audit risk,
lowers administrative burden,
and supports stable provider networks.
Commercial Plan Realities
Commercial plans prioritize:
Utilization management efficiency
Predictable audit outcomes
Network adequacy and retention
Reduced administrative cost
Clear documentation standards
SMART charting has been used as a proxy for accountability, but it often unreliable.
Why SMART Charting Increases Cost
In outpatient psychotherapy, SMART charting:
Produces lengthy, inconsistent narrative notes
Requires significant reviewer interpretation
Leads to higher rates of audit disagreement
Drives provider dissatisfaction and network exit
This increases both direct administrative cost and indirect access risk.
How the GRID Improves Commercial Plan Outcomes
The GRID benefits commercial plans by:
Providing standardized, interpretable records
Reducing variability in documentation quality
Supporting faster, cleaner utilization review
Lowering appeal and grievance rates
Improving provider satisfaction and retention
GRID records answer the question reviewers actually ask:
“What was done, why, and did it work?”
Commercial Plan Bottom Line
The GRID delivers the accountability commercial plans seek—with lower administrative cost, fewer disputes, and stronger networks—without requiring SMART narrative compliance.
Final Cross-Payer Statement
Across Medicare, Medicaid, OHP, and commercial plans:
SMART charting is a third-generation administrative heuristic.
The GRID is a fourth-generation outpatient psychotherapy documentation system.
The GRID captures SMART attributes inherently, while also delivering:
higher reliability,
stronger audit defensibility,
better privacy protection,
and greater workforce sustainability.
References
American Counseling Association. (2024). Guidance on ethical use of AI and digital tools in counseling practice. American Counseling Association.
https://www.counseling.org/knowledge-center/ethics/artificial-intelligence
American Psychological Association. (2007). Record keeping guidelines.
https://www.apa.org/practice/guidelines/record-keeping.pdf
American Psychological Association. (2025). Ethical guidance for AI in practice. American Psychological Association. https://www.apa.org/monitor/2023/11/ethics-artificial-intelligence
Blueprint. (2025). Behavioral health EHRs: What’s working, what’s broken, what’s next. Blueprint.
https://www.blueprint.ai/blog/behavioral-health-ehrs-whats-working-whats-broken-whats-next
Centers for Medicare & Medicaid Services. (2014). Medicaid documentation for behavioral health practitioners (ICN 909160). https://www.cms.gov/medicare-medicaid-coordination/fraud-prevention/medicaid-integrity-education/downloads/docmatters-behavioralhealth-factsheet.pdf
Documentation Wizard. (2024). Challenges and risks of AI-assisted progress notes in psychotherapy documentation. Documentation Wizard.
https://documentationwizard.com/challenges-with-ai-in-progress-notes/
Doran, G. T. (1981). There’s a S.M.A.R.T. way to write management’s goals and objectives. Management Review, 70(11), 35–36. https://community.mis.temple.edu/mis0855002fall2015/files/2015/10/S.M.A.R.T-Way-Management-Review.pdf
Eleos Health. (2020). Behavioral health clinicians are drowning under a pile of paperwork. Eleos Health.
https://eleos.health/blog/behavioral-health-clinicians-are-drowning-under-a-pile-of-paperwork/
ICD10monitor. (2025). Why AI-generated notes pose the same risks as chart cloning. ICD10monitor.
https://icd10monitor.medlearn.com/why-ai-generated-notes-pose-the-same-risks-as-chart-cloning/
Independent Mental Health Practices Alliance & Mentor Research Institute. (2021).
Psychotherapy treatment plans and progress notes can have chilling effects. Policy and analysis materials.
https://www.imhpa.org/charting-chilling-effect-on-patients-outcomes
King, M. G. (2014). Clinical record keeping in psychological practice – complete, accurate, ethical? Journal of Law and Ethics, 5(1). https://static1.squarespace.com/static/5449b8f8e4b07f67352573bb/t/60c3b21e7a9117324a31fc25/1623437855536/CLINICAL%2BRECORD%2BKEEPING%2BIN%2BPSYCHOLOGICAL%2BPRACTICE%2B%2BComplete%2BAccurate%2BEthical.pdf
Lewis, C. C., Boyd, M., Puspitasari, A., Navarro, E., Howard, J., Kassab, H., Hoffman, M., Scott, K., Lyon, A., Douglas, S., Simon, G., & Kroenke, K. (2019). Implementing measurement-based care in behavioral health: A review. JAMA Psychiatry, 76(3), 324–335. https://pubmed.ncbi.nlm.nih.gov/30566197/
Mentor Research Institute. (2023). What is the value of psychotherapy charting in practice?
https://www.mentorresearch.org/value-psychotherapy-charting
Mentor Research Institute. (2025). What is the value of psychotherapy charting in practice?
https://www.mentorresearch.org/value-psychotherapy-charting
Mentor Research Institute. (2025). What is the value of psychotherapy charting in practice?
https://www.mentorresearch.org/value-psychotherapy-charting
Shanafelt, T. D., Dyrbye, L. N., Sinsky, C., Hasan, O., Satele, D., Sloan, J., & West, C. P. (2016). Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clinic Proceedings, 91(7), 836–848.
https://pubmed.ncbi.nlm.nih.gov/27313121/
U.S. Department of Health & Human Services. (2017). HIPAA and mental health information: Extra protections and psychotherapy notes.
https://www.hhs.gov/hipaa/for-professionals/special-topics/mental-health/index.html